Services
Medical Billing
Ensure accurate claim submission and faster reimbursements.
Medical Coding
Apply correct codes for error-free claim approvals.
Provider Credentialing
Get providers enrolled with payers smoothly and quickly.
Insurance Verification
Confirm patient coverage before services to reduce denials.
Patient Scheduling
Organize appointments efficiently for better practice workflow.
Denial Management
Identify, correct, and resubmit denied claims effectively.
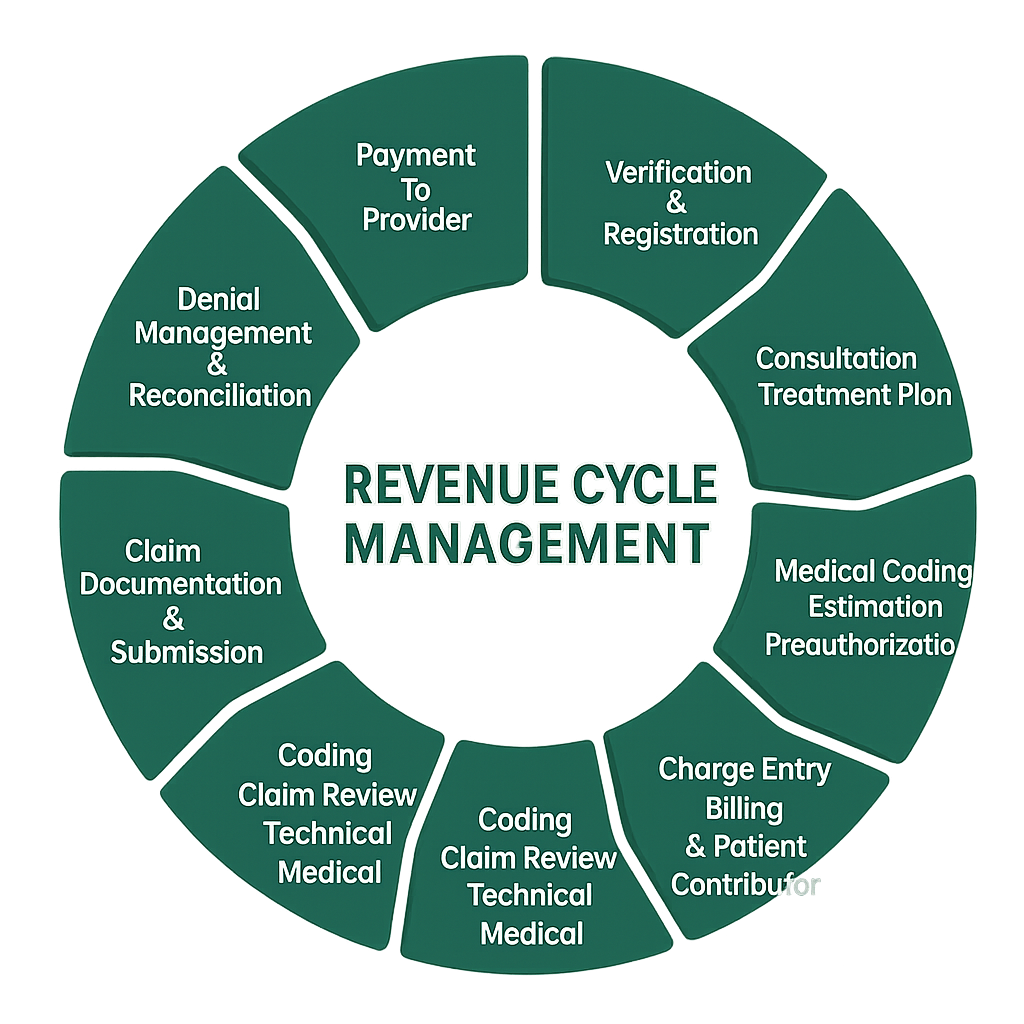
Revenue Cycle Management
End-to-end billing process for steady cash flow.
Front Office Support
Assist patients with billing clarity and payment ease.
GET A FREE CONSULTATION
330 470 8452
Have questions about your practice billing? Just give us a call and get a free consultation today.
Our Workflow
Why Choose Us for Medical Billing Services?
We provide medical billing and credentialing services tailored for healthcare practices, helping maximize revenue, cut denials, and stay compliant with regulations.
- Maximized Revenue
- Streamlined Credentialing
- Clear Communication
- Hipaa Compliance
Medical Billing Services
Handling medical billing in-house can be stressful and lead to delayed payments. Claim submissions, follow-ups, and denials often distract you from patient care.
Our team manages the entire process — from accurate claim filing to payment posting — ensuring faster reimbursements and fewer errors. You stay focused on your patients while we keep your revenue cycle smooth.


Medical Coding Services
Incorrect coding can lead to claim denials, revenue loss, and compliance issues. Managing it in-house can be time-consuming and prone to errors.
Our expert coders ensure accurate, compliant coding for every claim, reducing denials and speeding up reimbursements. We make coding simple so you can focus on patient care with confidence.
Documentation & Verification
Collect and verify provider documents within 7–10 days.
Licensing Submission
Prepare and submit licensing applications within five business days.
Follow-Up Reporting
Provide weekly progress reports and status updates to stakeholders.
Credentialing Review
Manage payer reviews and enrollment within 60 business days.
Contracting & Onboarding
Negotiate contracts and complete onboarding within 90 business days.
Provider Credentialing
Credentialing can be a complex process that delays provider onboarding and impacts revenue. Handling documents, applications, and follow-ups often takes focus away from patient care.
Our team manages the entire process — documentation, licensing, follow-ups, credentialing, and contracting — ensuring everything is completed accurately and on time. We keep you updated so you can focus on growing your practice with confidence.

Revenue Cycle Management
Manual insurance checks can slow operations and cause claim denials. We verify patient coverage in advance so you can focus on care, not paperwork.
- Patient registration and insurance verification
- Accurate charge capture and claim submission
- Denial management and appeals
- Payment posting and reconciliation
- Detailed financial reporting and insights
Front Office Support
Managing calls, appointments, and patient inquiries can take valuable time away from your staff. Our front office support team ensures smooth communication and a professional experience for every patient.

Insurance Verification
Insurance verification errors can lead to claim denials, delayed payments, and extra administrative work. Manually checking coverage slows down your team and takes the focus away from patient care.
Our team verifies eligibility, benefits, deductibles, and co-pays before each appointment to ensure accurate claims and faster reimbursements. With proper verification, you minimize denials and keep your cash flow consistent.
Patient Scheduling
Managing appointments manually can cause double-bookings, missed visits, and wasted time. This disrupts your staff’s workflow, reduces provider productivity, and creates a poor patient experience.
Our team manages scheduling, confirmations, reminders, and cancellations to keep your calendar organized and minimize no-shows. With smooth scheduling, your practice runs efficiently and patients have a better experience.

Identify Denials
Analyze rejected claims and categorize issues
Correct Errors
Fix coding, eligibility, or documentation mistakes
Resubmit Claims
Quickly correct and resubmit for fast payment
Track Trends
Monitor patterns to prevent repeat denials
Optimize Process
Improve workflows to reduce future claim issues
Denial Management
Effective denial management is crucial for protecting your practice’s revenue and ensuring a healthy cash flow. When claims are denied, payments get delayed, and your staff spends extra time fixing errors and resubmitting claims.
Our streamlined process helps recover lost revenue faster, minimizes disruptions, and prevents future denials by addressing the root cause of each rejection.
